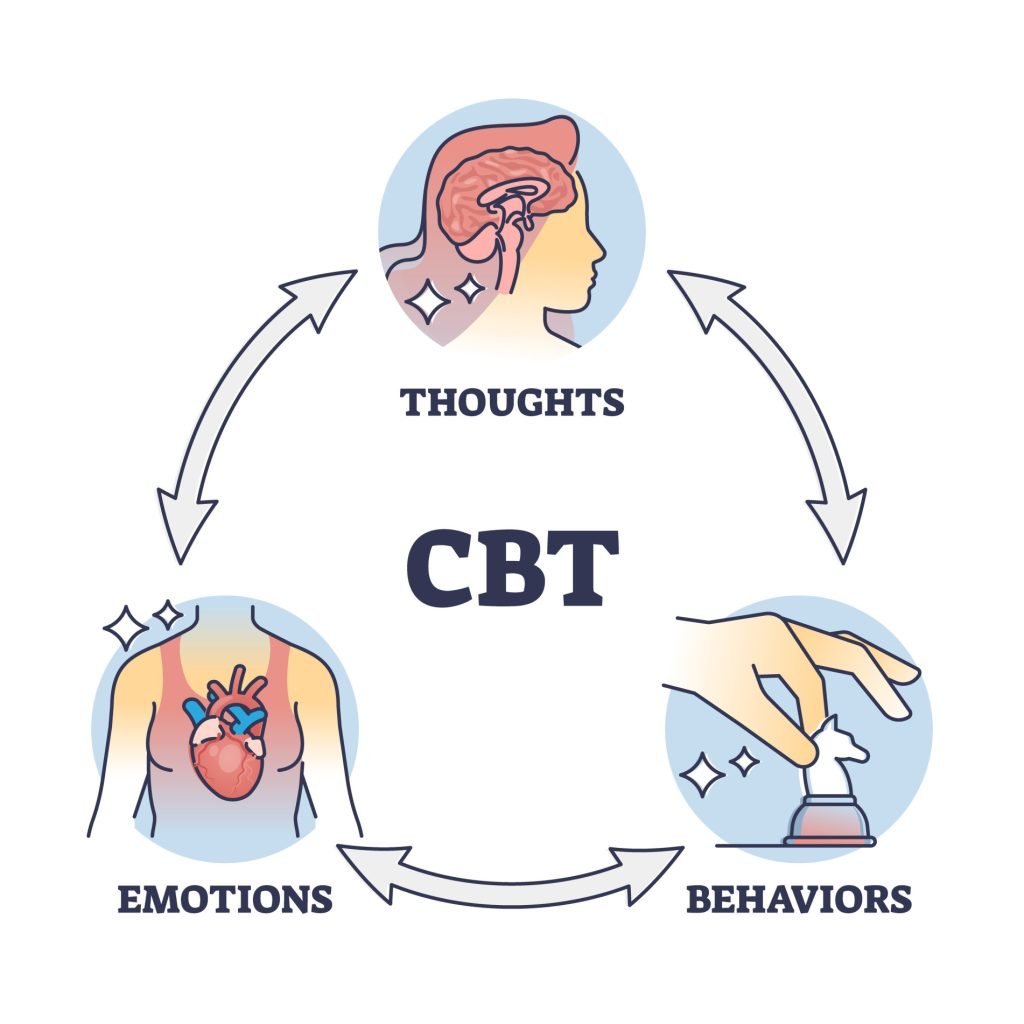
Cognitive behavioral therapy (CBT) is an evidence-based form of psychotherapy that focuses on the connections between thoughts, emotions, and behaviors. It aims to improve mental health issues by targeting unhelpful thinking patterns and maladaptive actions.
CBT has been used to effectively treat conditions like depression, anxiety, eating disorders, and more recently, attention-deficit/hyperactivity disorder (ADHD).
ADHD is a common neurodevelopmental disorder characterized by difficulties with inattention, hyperactivity, and impulsivity that cause impairment in daily functioning.
Both psychosocial and medication treatments can help manage ADHD symptoms. CBT provides personalized strategies to better regulate behavior and optimize brain function.
This article will examine how the CBT approach is well-suited to addressing the core difficulties faced by individuals with ADHD.
Applying CBT Theory to ADHD
In CBT, past experiences, especially during childhood and adolescence, play an important role in shaping our deeply held beliefs and rules about ourselves, others, and the world.
These beliefs go on to influence how we think, feel, and act in current situations.
For ADHD, certain difficult developmental experiences related to inattention, disorganization, emotional volatility, or difficulty following rules can form negative beliefs like “I’m incapable of completing tasks properly” or “I’m incompetent.” Facing repeated academic failures or relationship problems because of ADHD symptoms can also lead to beliefs of being defective.
Such beliefs often lead to unhelpful compensatory strategies which represent attempts to protect oneself but end up being self-defeating. For example, someone might avoid taking on responsibilities out of fear that others will be upset by mistakes, even though this avoidance leads to criticism for being unreliable.
Understanding these connections informs the CBT treatment approach.
CBT Model of ADHD
There are several key premises that describe the nature of ADHD and guide psychosocial CBT interventions:
- ADHD lies at the extreme end of normal self-regulation problems: While ADHD symptoms lead to clinically significant impairment, they exist on a continuum of executive functioning deficits seen in all individuals to varying degrees.
- ADHD directly causes functional impairment: Inattention, hyperactivity, and impulsivity interfere with effectively performing tasks and responsibilities required for normal daily activities.
- ADHD undermines personal goals and efficacy: The inability to consistently implement plans despite otherwise viable goals leads to reduced confidence in one’s capabilities and effectiveness.
- ADHD affects social belonging: Repeated failures over time can strain relationships with friends, family, coworkers, etc.
- ADHD influences information processing: Negative thoughts and beliefs develop in response to ADHD-related frustrations, and these thoughts perpetuate difficulties by justifying avoidance and disengagement.
Clinical Implications
The CBT approach views ADHD as primarily a difficulty of being unable to implement the skills needed to achieve goals, not an inability to learn those skills. For example, even though individuals with ADHD understand the value of keeping a planner, they struggle to consistently maintain one.
CBT targets multiple areas of functioning affected by ADHD:
Cognitive: Identify and dispute counterproductive thoughts that exacerbate struggles to build motivation and efficacy
Behavioral: Personalize organizational systems and planning tools to improve follow-through
Emotional: Learn to better tolerate the discomfort/boredom of essential responsibilities
Implementation: Use prompts, rewards, accountable partnerships to bridge the intention-action gap
Social: Practice expressing needs assertively and negotiating roles to improve relationships
A strong therapeutic alliance also provides needed support and encouragement during the challenging process of behavior change.
Targeting ADHD Difficulties
CBT for ADHD involves learning personalized strategies to compensate for executive functioning deficits in the domains of time management, organization, planning, attention regulation, restraint from impulsive actions, and emotion control.
As an example, for the executive function of working memory, which involves holding information in mind and using it to guide actions, CBT targets identifying external memory aids. This might include using visual reminders, alarms, checklists, and breaking down larger tasks.
CBT would also address the discouraging thoughts that arise when one’s system fails, such as “I can’t even remember to do basic things, I’m so stupid.”
Through discussion, the client is helped to generate more accurate and helpful thoughts like “I struggled with this due to my ADHD challenges. Now I know ways I can adapt to support my memory.”
Emotion regulation is another common target, as emotional impulsiveness leads individuals with ADHD to overreact, express anger inappropriately, or engage in reckless behaviors. CBT helps clients to identifiy the triggers ahead of time, use calming strategies in the moment, evaluate the consequences of actions, and build distress tolerance.
Across these areas, CBT uses behavioral experiments to test out new strategies and determine what works best for each individual’s needs.
CBT Techniques for ADHD
CBT incorporates several methods to address unhelpful cognitions and behaviors:
- Cognitive restructuring: Identifying automatic negative thoughts when frustrated, evaluating their accuracy, and coming up with alternative interpretations
- Behavioral activation: Strategically scheduling pleasurable activities to lift mood and boost motivation for responsibilities
- Problem-solving training: Breaking larger tasks down into smaller actionable steps
- Stimulus control interventions: Removing distractions to focus attention and using triggers to remember actions
- Exposure therapy: Gradually confronting feared tasks to reduce avoidance
CBT also aims to build key skills like organization, planning, prioritization, and time management by trying different systems to find an optimal individual fit. This includes using physical tools like whiteboards, planners, and daily to-do task lists.
Developing routines around sleep, meals, exercise, and other basic self-care activities is also important. Accountability measures like shared calendars and check-ins can enable progress tracking.
Emotion regulation techniques help clients better understand their feelings, tolerate uncomfortable emotions, and moderate impulsive reactions. These include journaling moods to identify triggers, relaxed breathing, counting before responding, and thinking through the consequences of different responses.
Such strategies aim to improve self-efficacy – one’s belief in their ability to carry out actions and reach goals. By targeting small, specific problems and building skills through regular practice, CBT facilitates tangible gains in functioning that translate into improved self-confidence.
The Therapist-Client Relationship
The therapist–client relationship lies at the heart of CBT’s success. Through expressing empathy, validating clients’ experiences, instilling hope, and using collaborative approaches, therapists help clients feel understood and empowered. This motivates engagement in the challenging work involved in countering lifelong maladaptive habits.
CBT is an active treatment that expects clients to apply learned techniques between sessions while monitoring and reporting outcomes.
Therapists provide psychoeducation, model new skills, role-play scenarios, share resources, make referrals, and hold clients accountable. Finding optimal ways to incentivize and enable behavior change is an iterative, customized process.
Why CBT May Not Always Work
Although CBT is considered an evidence-based psychosocial treatment for ADHD in adults, it may not always be effective or the best choice for everyone.
So why might CBT not fully alleviate ADHD difficulties for some individuals?
First, ADHD has underlying neurological underpinnings that cannot be eliminated through psychosocial means, even if compensated for.
Additionally, CBT mainly targets volitional aspects of mental functioning that are consciously accessible. Less amenable unconscious processes require alternative therapies.
The need to actively and consistently apply learned techniques can also prove challenging for clients struggling with follow-through. Access and cost barriers may impede engagement.
Other complementary approaches include mindfulness to build attentional control and awareness, cognitive remediation therapy focusing on basic information processing capacities, and occupational therapy for daily living skills.
Combined treatment modalities address different facets of impairment for more comprehensive management. Support groups provide community belonging and inspiration. Overall, multifaceted treatment accounting for individual preferences and life context is key for adults with ADHD.
Conclusion
In conclusion, CBT offers a practical approach for helping those with ADHD strengthen their self-regulatory capacities and minimize associated life impediments.
The cognitive conceptualization of ADHD provides a framework for understanding its daily impacts.
Highly tailored behavioral strategies target establishing constructive habits and routines. Attention to negative thought patterns alleviates their obstruction to motivation and success.
A supportive therapeutic relationship facilitates progressive gains in functioning.
Implementing CBT techniques requires commitment but can greatly improve quality of life for adults with ADHD.
CBT may not work for every aspect of ADHD in adults and it is advisable to incorporate a multifaceted approach when managing a neurodiverse condition.
References
Beck, A. T., & Haigh, E. A. (2014). Advances in cognitive theory and therapy: The generic cognitive model. Annual review of clinical psychology, 10, 1-24.
Dobson, K. S., Poole, J. C., & Beck, J. S. (2018). The fundamental cognitive model. Science and practice in cognitive therapy: Foundations, mechanisms, and applications, 29-47.
Miklósi, M., Máté, O., Somogyi, K., & Szabó, M. (2016). Adult attention deficit hyperactivity disorder symptoms, perceived stress, and well-being: the role of early maladaptive schemata. The Journal of Nervous and Mental Disease, 204(5), 364-369.
Ramsay, J. R. (2020). Rethinking adult ADHD: Helping clients turn intentions into actions. American Psychological Association. https://doi.org/10.1037/0000158-000


