Attention-deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental disorder typically diagnosed in childhood that often persists into adolescence and adulthood. The core symptoms of ADHD include inattention, hyperactivity, and impulsivity, which interfere with functioning and development across multiple domains.
About 5-7% of school-age children and 4% of adults meet diagnostic criteria for ADHD. However, many more individuals struggle with impairing attention difficulties and hyperactive/impulsive behaviors that impact their daily lives.

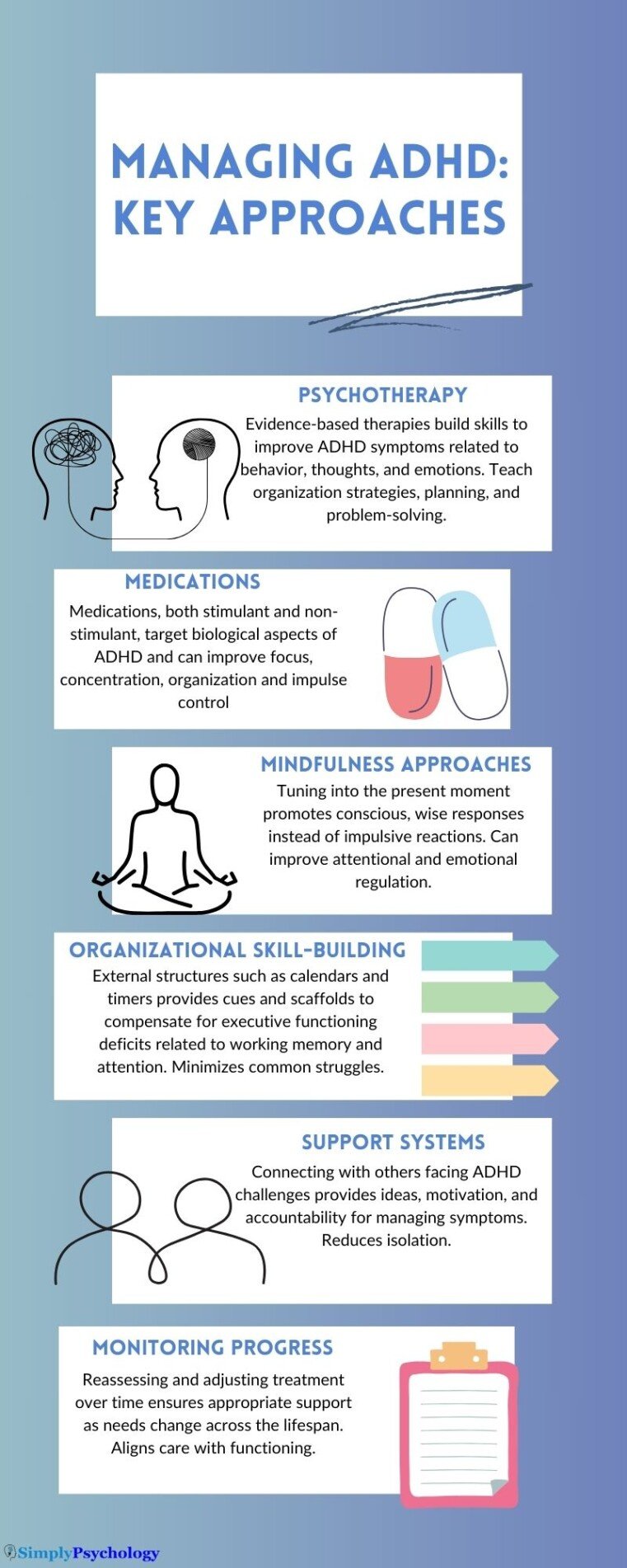
Effective treatment is crucial for managing impairing ADHD symptoms that interfere with personal, social, academic, and occupational functioning across the lifespan, such as emotion dysregulation, mood swings, and executive dysfunction.
This article provides an overview of evidence-based pharmacological and non-pharmacological treatments for ADHD as well as monitoring considerations and special patient populations requiring unique treatment approaches.
Medication
Stimulant medications are recommended as part of first-line ADHD treatment for children (ages 6+), adolescents, and adults under the care of a medical provider (although they can come with side effects and may not be suitable for everyone).
Stimulants target biological aspects of ADHD by increasing the availability of the neurotransmitters dopamine and norepinephrine in the brain to improve concentration, organization, productivity, and impulse control.
When selecting a stimulant, factors like speed of desired symptom relief, duration of action needed to cover daytime hours of highest impairment, mode of delivery (tablet, patch, liquid), likelihood of compliance, potential adverse side effects, and abuse risk (for adults or adolescents) help determine the most appropriate medication and dosage schedule for each patient’s needs.
Types of Stimulant Medications
Methylphenidate-Based Stimulants
- Ritalin/Methylin – immediate release tablet, lasts about 4 hours
- Concerta/Jornay – extended release capsule, lasts 10-12 hours
- Daytrana – transdermal skin patch changed daily
- Fast-acting focalin/Ritalin may supplement long-acting doses
Dextroamphetamine-Based Stimulants
- Dexedrine/Zenzedi/Evekeo – tablet, lasts about 5 hours
- Adderall/Mydayis – mixed amphetamine salts, immediate (Adderall) or extended-release capsule (Adderall XR, Mydayis)
- Vyvanse – prodrug stimulant converted in the body, lasts over 8 hours
- Dyanavel/Procentra – liquid, lasts 4+ hours
Benefits of Stimulant Medication
- Improve core symptoms – enhanced focus, concentration, organization
- Increase impulse control and reduce hyperactivity
- Boost learning, academic productivity and test performance
- Improve driving ability and reduce risk of accidents
Potential Adverse Effects
Most common: Decreased appetite, headaches, irritability, insomnia, cardiovascular effects – often dose-dependent and diminish over time for most patients. Rare risks require prompt medical care like prolonged painful erections or suicidal thoughts during early treatment.
Non-Stimulant Medications
These medications have a different mechanism of action but also target biological components of ADHD. If prescribed, they must be taken daily long-term to maintain symptom relief.
Options include:
- Atomoxetine – selective norepinephrine reuptake inhibitor
- Guanfacine, clonidine – activate alpha2 receptors in prefrontal cortex
- Viloxazine – selective norepinephrine reuptake inhibitor
- Bupropion – norepinephrine-dopamine reuptake inhibitor; off-label
Around 30% of those with ADHD have limited response to stimulants but experience a reduction in ADHD symptoms from non-stimulants. These medications may also be combined with stimulants or used alone when stimulant treatment is ineffective/problematic.
Benefits
- Provide alternative treatment or supplement stimulants
- Extended coverage – 24-hour action for symptoms persisting after stimulants wear off
- Lower abuse potential
Potential Adverse Effects
Sedation, headaches, irritability, gastrointestinal symptoms – often diminish over time. Rare risks of liver injury or suicidal thoughts during early treatment require prompt medical care. Gradual taper of these medications reduces complications if discontinued.
Before considering medication options, please discuss your options and the full side effects with a health professional. This article is meant only as a summary of medications and should not be taken as medical advice.
Psychotherapy
Various types of therapy and support teach individuals with ADHD new skills to directly improve their psychological and behavioral regulation.
These interventions address aspects of impairment related to underlying ADHD neurobiology but not targeted by medication treatment alone. Parent training is also included for managing children with ADHD.
Cognitive-Behavioral Therapy
Cognitive-behavioral therapy (CBT) for ADHD helps identify and shift negative thinking patterns like “I just can’t focus, nothing will help,” which exacerbates ADHD struggles.
Reconstructing self-defeating thoughts builds confidence to apply new skills taught in CBT like:
- Organizational systems – planners, electronic alerts, labeling, file management
- Time management – breaking down tasks, scheduling focused work intervals
- Planning/prioritizing – short and long-term goal setting, task analysis
- Self-monitoring – focus rating scales, assessing own attention and performance
- Problem-solving – evaluating challenges systematically then developing action plans
Both individual and group CBT improve core symptoms, emotional regulation, productivity, motivation and life satisfaction in various ADHD populations.
A meta-analysis examining 28 studies indicates CBT effectively reduces both core ADHD symptoms (inattention, hyperactivity, impulsivity) and emotional symptoms like anxiety and depression in adults with ADHD.
Considerations:
- Can be time-consuming to implement organizational systems and new habits. Dropping out due to feeling overwhelmed is a risk.
- Focusing extensively on changing thoughts could increase masking behaviors or emotional inhibition. Assessing ongoing internal experiences is important.
Dialectical Behavior Therapy
Dialectical behavior therapy (DBT) blends CBT with mindfulness exercises and emotional coping tactics from Zen Buddhist traditions using concepts of radical acceptance and tolerating distress.
DBT provides psychological skills training in four areas:
- Mindfulness – nonjudgmental focus on the present moment
- Distress tolerance – coping ahead and in the moment with strong emotions
- Emotion regulation – identifying and modifying reactions
- Interpersonal effectiveness – maintaining self-respect and relationships
Research indicates DBT improves ADHD symptoms along with emotional impulsivity and may be particularly helpful for adults with co-occurring mood disorders and suicidal ideation.
Considerations:
- Radical acceptance may excuse harmful behaviors without accountability. Needs balance with change.
- Mindfulness could enable avoidance of necessary life responsibilities/demands instead of building coping skills.
Behavior Therapy Techniques
Parents, teachers and medical providers can be trained to implement these strategies:
- Positive reinforcement and rewards to strengthen desired behaviors
- Appropriate negative consequences for problematic behaviors
- Removing triggers and tailored accommodations
Methods aim to motivate individuals with ADHD using frequent feedback matched to their struggles with delayed reinforcement from consequences as well as facilitating environmental supports.
Common behavior therapy programs include:
- Parent Training – Teaching parenting skills and behavior modification tailored to child/teen ADHD issues improves conduct across home and school settings. Particular focus on promoting consistency with discipline and social/academic development.
- Classroom Management – Trains teachers in providing structured limits, redirection of disruptive ADHD behaviors and reinforcement delivery through daily report cards tied to personalized behavioral goals students work towards.
- Child Skills Training – Direct coaching for kids/teens to boost organizational abilities, social skills pragmatics and self-control with bridging delays to reinforcement. Best results come from practicing these abilities across natural settings.
Considerations:
- Over-reliance on external reinforcement can prevent developing intrinsic motivation and discipline.
- Strict adherence to rewards/consequences often proves unrealistic long-term. Can’t control all environments.
Other Interventions
Other non-pharmacological options for coping with ADHD impairment continue emerging, though more research is needed to confirm their efficacy and feasibility for widespread use.
Mindfulness interventions
Dr. Dawn-Elise Snipes explains how mindfulness training can be helpful for improving ADHD symptoms and executive functioning deficits.
She notes that mindfulness interventions that encourage individuals to slow down, be more thoughtful, and tune into the present moment showed improvements in attention regulation, impulse control, organization, and emotional dysregulation.
Often, mindfulness training will incorporate environmental cues or triggers to remind the ADHD individual to check in with themselves and consciously choose skillful responses instead of acting on autopilot. For example, setting cell phone alerts for short mindfulness breaks.
Additionally, mindfulness involves self-awareness of which environments and situations bring out the best versus worst in symptoms. Dr. Snipes gives the example of her son choosing study spots carefully to limit distracting stimuli and optimize his concentration abilities.
Being mindful of your personal rhythms, energy levels, peak performance times, and early warning signs that attention or focus is declining can also be very strategic. Then, the individual can take timely breaks or switch tasks proactively.
The key premise behind using mindfulness for ADHD is to promote conscious choices and wise responses instead of impulsive, habitual reactions.
Customizing the training to the individual’s unique symptoms and challenges is important, as is starting small with reasonable expectations for someone with executive functioning deficits.
Neurofeedback
Uses displays of brain activity patterns from scalp electrodes, often presented as video games that challenge ADHD patients to alter the feedback by sustaining attentional control.
Success in practicing self-regulation of brain waves may then reinforce similar attention skills in daily life.
Some evidence shows ADHD symptom reduction but little data confirms functional or persisting gains from neurofeedback.
Dietary Supplements
Certain vitamins, minerals and amino acids affect neurotransmitter systems linked to ADHD impairment.
Daily iron, zinc, magnesium, omega-3s or S-adenosylmethionine (SAMe) supplementation demonstrates potential as safe ADHD interventions yet requires further study to specify efficacy and proper dosing.
Physical Activity
Aerobic exercise elevating heart rate prompts the release of neurotransmitters that influence ADHD abilities for concentration, cognitive flexibility, and mood stability.
Frequent running/activity breaks may improve classroom behavior in students with ADHD, likely by increasing task salience afterward. Going to the gym during the daytime may also alleviate restlessness at work for many individuals.
Sleep Hygiene
Many with ADHD suffer co-occurring sleep disturbances that worsen daily symptoms. Getting adequate quality restorative sleep sustains attention, memory, and emotional regulation impaired in ADHD.
Optimizing sleep boosts treatment outcomes, too, by enhancing medication efficacy, therapy receptiveness, and physical activity tolerance.
Building Organizational Skills
Dr. Dawn-Elise Snipes explains how organizational skills can be helpful for managing ADHD symptoms like inattention, distractibility, and executive functioning challenges.
She notes that research has found that explicitly teaching organizational skills leads to moderate improvements in ADHD issues.
Some examples of helpful organizational strategy training include using checklists, setting up systems and designated homes for important items, and creating assignment templates or frameworks.
For instance, having a special box, basket, or “launch pad” area for keys, bags, phones and other essentials when entering the house can assist with memory, planning ahead, and losing track of items.
Checklists for backpacks, projects, grocery shopping, and more can help compensate for working memory and attention lapses by providing an external cue system. Assignment rubrics that outline each component required can act as a scaffold for breaking down complex tasks.
The rationale is that by building habits, routines, and structural supports, many common ADHD-related frustrations around organization, follow-through, and forgetfulness can be minimized. This, in turn, alleviates self-esteem issues and motivational problems and reduces family tensions.
The key is to customize the strategies to the individual’s unique needs and difficulties. Organizational skills training aims to set the person up for success instead of highlighting deficits. It provides the scaffolding and tools to bypass neurological weaknesses.
ADHD Support Groups
ADHD support groups connect individuals facing similar struggles, reducing isolation. Sharing personal experiences and successful strategies provides motivation and ideas for practical symptom management.
Groups foster accountability through encouragement and empathy from those managing the same disorder and understanding ADHD’s impact. This motivates persevering with treatments and builds self-compassion.
Treatment Planning and Monitoring
Performing comprehensive assessments across domains of impairment guides developing individualized ADHD management plans while monitoring response. Follow-up care adjusts approaches over time for chronic, progressive treatment.
Selecting Appropriate Initial ADHD Services
Input from patients, parents, teachers, and medical experts identifies:
- Symptom severity, presentation, and comorbidities requiring care
- Extent medication being prescribed improves daily functioning
- Specific abilities requiring psychological or academic assistance
- Resources available within families/schools supporting new skills
These factors shape what services start treatment – often medication and/or training for parents and teachers in proven ADHD behavior strategies.
Monitoring Progress Over Time
Frequent check-ins following ADHD treatment initiation determine:
- Any medication adjustments needed for tolerability or efficacy
- Emerging side effects or adherence issues requiring intervention
- How well implemented therapeutic techniques work applied independently
- Whether learned skills successfully generalize across settings
Changes should align treatments better with shifting needs from neurodevelopment, life transitions or new impairments manifesting over time.
Promoting Generalization and Maintenance
For lasting benefits, individuals with ADHD continually apply trained strategies and perform emergent skills in natural environments like:
- Using planners and to-do lists for organizing/meeting deadlines at school and home
- Practicing conversing without interruptions among different friend groups
- Taking medication daily as prescribed despite no immediate external accountability
Reinforcement from experiencing self-efficacy and natural rewards for success help new ADHD-targeted behaviors endure so supports can fade.
Special Considerations
Unique factors shape ADHD treatment for patients of different ages, supporting the need for specialized care across the lifespan tailored to each population’s needs.
Preschool Kids
Distinct diagnostic challenges in differentiating neurotypical childhood activity from ADHD symptoms in this group mean medication is rarely prescribed. However, behavioral difficulties can be addressed effectively through early intervention.
Common Preschool ADHD Treatment Elements:
- Parent training in developmentally appropriate expectations and responses along with accommodating structure and routines amid kids’ shifting abilities
- Encouraging play with peers and adults to build social skills
- Fostering language and self-regulation growth
Adolescents
Pubertal changes interact uniquely with ADHD challenges emerging as expectations increase for older students. Assessment should determine if previous accommodations still help overcome current barriers.
Common Adolescent ADHD Treatment Elements:
- Study/organization skills training for handling workload/pace complexity
- Driving readiness assessments regarding risk-taking behaviors
- Substance misuse prevention education amid impulse control difficulties and peer exposure
Adults
Symptoms often resemble childhood history but require updated screening. Stigma delays many adults from seeking help despite significant impairment.
Common Adult ADHD Treatment Elements:
- Psychotherapy for inadequate coping abilities and chronic functional complications
- Couples counseling to enhance communication and relationship preservation
- Job coaching and workplace accommodations provide support without drawing negative attention
- Medication prescribed/monitored carefully due to greater misuse risk
Older Patients
Distinguishing lifelong ADHD from new attentional deficits in older ages proves difficult. Emotional dysregulation and sleep disturbances should be managed too.
Common Treatment Considerations for Older Patients with ADHD History:
- Reviewing onset timing and symptom course plus collateral history to confirm diagnosis
- Adjusting medication cautiously due to higher adverse effects and drug interaction likelihood
- Advising on elevated medical risks requiring diligent monitoring
Conclusion
In summary, ADHD is a common neurodevelopmental disorder often causing substantial lifelong impairment, but evidence-based treatment tailored to each patient’s needs helps manage symptoms and skill deficits interfering with optimal functioning.
The most robust treatment response usually comes from combining pharmacological and behavioral approaches to respectively target biological and developmental aspects of ADHD in a coordinated multimodal care plan.
Still, given the considerable heterogeneity observed in ADHD clinical presentations, treatment tolerance/response and access among various populations, highly individualized ongoing assessments should always guide delivery of interventions and services.
Treatment planning must consider developmental stage, symptom profiles, co-occurring conditions, and available supports to successfully address one’s current daily obstacles related to ADHD while also helping build lifelong self-efficacy in managing persistent struggles.
Though no cure exists, consistent, dedicated treatment teaches individuals with ADHD how to minimize their disorder’s disruption across all facets of life – learning, working, parenting, relationships, and health management.
Care must be taken with ADHD management that individuals are not being encouraged to simply mask their symptoms of ADHD, which in itself can come with issues. People with ADHD should be encouraged to be authentically themselves while also working towards their specific goals and taking accountability for their actions.
Researchers build on growing insights about ADHD’s precise neurobiological and genetic underpinnings to keep improving diagnostic accuracy and expanding treatment possibilities for patients along the lifespan journey with ADHD.
References
Abootorabi Kashani, P., Naderi, F., Safar Zadeh, S., Hafezi, F., & EftekharSaadi, Z. (2020). Comparison of the effect of dialectical behavior therapy and emotion regulation on distress tolerance and suicide ideation in symptoms of attention deficit/hyperactivity disorder in adolescents. Psychological Achievements, 27(2), 69-88.
Daley, D., van der Oord, S., Ferrin, M., Danckaerts, M., Doepfner, M., Cortese, S., & Sonuga-Barke, E. J. (2014). Behavioral interventions in attention-deficit/hyperactivity disorder: a meta-analysis of randomized controlled trials across multiple outcome domains. Journal of the American Academy of Child & Adolescent Psychiatry, 53(8), 835-847. https://doi.org/10.1016/j.jaac.2014.05.013
Kaplan, G., & Newcorn, J. H. (2011). Pharmacotherapy for child and adolescent attention-deficit hyperactivity disorder. Pediatric Clinics, 58(1), 99-120. https://doi.org/10.1016/j.pcl.2010.10.009
Liu, C. I., Hua, M. H., Lu, M. L., & Goh, K. K. (2023). Effectiveness of cognitive behavioural‐based interventions for adults with attention‐deficit/hyperactivity disorder extends beyond core symptoms: A meta‐analysis of randomized controlled trials. Psychology and Psychotherapy: Theory, Research and Practice. https://doi.org/10.1111/papt.12455
Neef, N. A., Perrin, C. J., & Madden, G. J. (2013). Understanding and treating attention-deficit/hyperactivity disorder. In G. J. Madden, W. V. Dube, T. D. Hackenberg, G. P. Hanley, & K. A. Lattal (Eds.), APA handbook of behavior analysis, Vol. 2. Translating principles into practice (pp. 387–404). American Psychological Association. https://doi.org/10.1037/13938-015
Pfiffner, L. J., & Haack, L. M. (2014). Behavior management for school-aged children with ADHD. Child and Adolescent Psychiatric Clinics of North America, 23(4), 731-746. https://doi.org/10.1016/j.chc.2014.05.014
Rooney, M., & Pfiffner, L. J. (2018). Attention-deficit/hyperactivity disorder. In J. N. Butcher & P. C. Kendall (Eds.), APA handbook of psychopathology: Child and adolescent psychopathology (pp. 417–445). American Psychological Association. https://doi.org/10.1037/0000065-019
Safren, S. A., Sprich, S., Mimiaga, M. J., Surman, C., Knouse, L., Groves, M., & Otto, M. W. (2010). Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA, 304(8), 875–880. https://doi.org/10.1001/jama.2010.1192